Six months ago, I wrote a post called “When journal, scientific society, and community values clash.” I recounted the tale of the…
The post Six Months Later: What Their Response on ME/CFS Tells Us About the Cochrane Collaboration appeared first on Absolutely …
Why it matters
- The Cochrane Collaboration's response to criticism can influence future research practices and patient care standards.
- The handling of ME/CFS research illustrates the broader tensions between scientific rigor and community needs.
- Understanding these dynamics is crucial for stakeholders in health research and advocacy.
In a recent reflection on the ongoing discussions surrounding my previous article titled “When journal, scientific society, and community values clash,” I revisit the Cochrane Collaboration’s controversial stance on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Half a year ago, I highlighted the dissonance that emerged when scientific findings intersected with the deeply felt needs of the patient community. This reflection aims to dissect the implications of the Cochrane Collaboration’s responses and the broader lessons they reveal about the state of collaborative health research.
The Cochrane Collaboration, renowned for its commitment to evidence-based medicine, found itself at the center of a heated debate regarding its systematic review of ME/CFS treatments. Critics argued that the review not only overlooked significant patient experiences but also failed to adequately evaluate existing data on the condition. The backlash was swift and loud, echoing the sentiments of patients who have long felt marginalized within the medical community.
In the months following the publication of the review, the Cochrane Collaboration faced mounting pressure to address these concerns. Their initial responses were perceived by many as insufficient, failing to acknowledge the profound impact of ME/CFS on those affected by it. This response—or lack thereof—raised critical questions about the organization’s accountability and commitment to patient-centered research.
As advocates pushed for a re-evaluation of the review, the Cochrane Collaboration emphasized its dedication to transparency and scientific integrity. They committed to revisiting the review process and incorporating more diverse perspectives, including those of patients and advocacy groups. Such a commitment is a step in the right direction, but the effectiveness of this approach remains to be seen.
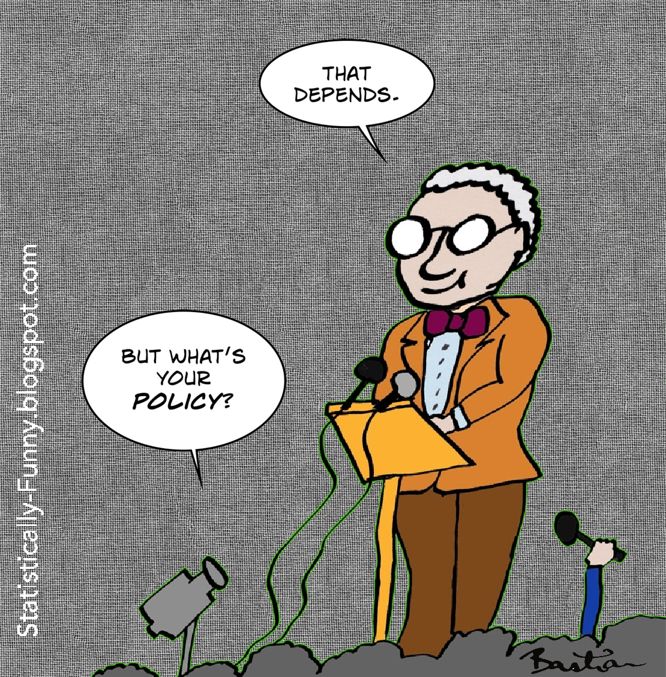
One notable aspect of this controversy is the tension between scientific objectivity and the lived experiences of individuals suffering from chronic illnesses. The Cochrane Collaboration has historically prided itself on rigorous methodology, but this rigor can sometimes come at the expense of the nuanced understanding that patient narratives can provide. In the case of ME/CFS, patients have long reported debilitating symptoms that are not easily quantifiable or understood through traditional research metrics. This disconnect highlights a critical flaw in the research process: the need for a more holistic approach that values patient input alongside empirical data.
Moreover, this situation underscores the importance of patient advocacy in shaping research agendas. The reaction from the ME/CFS community has been a clarion call for researchers to prioritize patient voices in their work. As more organizations recognize the significance of this approach, it could lead to a fundamental shift in how research is conducted and disseminated, allowing for more tailored and effective treatments for chronic illnesses.
The Cochrane Collaboration’s handling of this situation may serve as a pivotal moment for both the organization and the broader research community. If they can successfully integrate patient feedback into their review processes, it could establish a new standard for how chronic health conditions are studied and treated. On the other hand, failure to adequately address the concerns raised by the ME/CFS community could damage the organization's reputation and undermine its credibility in the eyes of both patients and researchers.
As the dialogue around ME/CFS continues, it is essential for all stakeholders to reflect on the implications of their actions and responses. The Cochrane Collaboration has an opportunity to lead by example, demonstrating how to balance scientific rigor with a compassionate understanding of patient experiences. This is not merely an academic debate; it is a matter of health equity and respect for those who navigate the complexities of chronic illness every day.
In conclusion, the response from the Cochrane Collaboration regarding ME/CFS is more than just a commentary on one specific condition. It is a reflection of the broader challenges within the scientific community as it grapples with the need for inclusivity and the integration of patient perspectives into research methodologies. As we move forward, it is crucial to ensure that the lessons learned from this experience inform future research practices, fostering a more collaborative and empathetic approach to health science.